A new study by a team of scientists Faculty of Health Sciences, the University of Nairobi and from multiple institutions in Kenya and the United States, led by James Mburu Kangethe (PhD Scholar from the Department of Medical Microbiology & Immunology and a CARTA Fellow), who is co-supervised by Dr. Stephen Gichuhi and Dr. Marianne Mureithi, offers crucial insights into the co-infection of high-risk Human papillomavirus (HR-HPV) and Human T-lymphotropic virus-1 (HTLV-1) among women living with HIV (WLHIV). The findings of this study underline the complexity of the public health landscape in Kenya, especially in relation to HIV and sexually transmitted infections.
Understanding the Co-infection
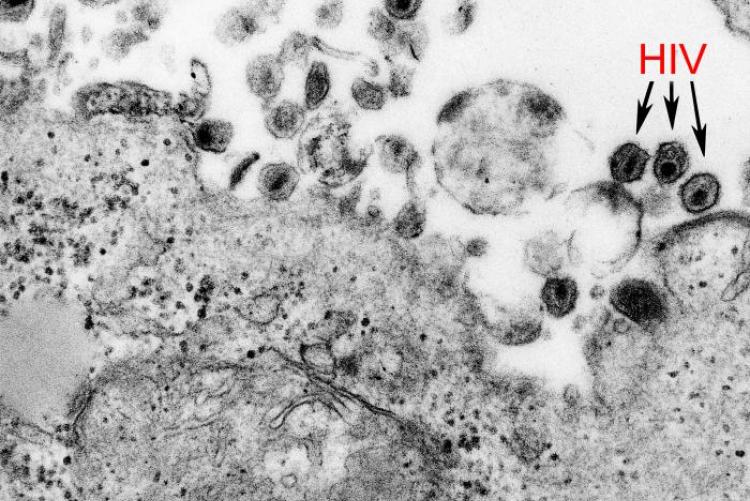
Globally, it is estimated that 15% of reported cancers are virus-associated. The implicated viruses include HR-HPV, which causes cervical cancer, and HTLV-1, which results in adult T-cell leukaemia (ATL). The retrovirus properties of HTLV-1 infection may enhance the susceptibility to acquiring HR-HPV infections, leading to a greater incidence of cervical abnormalities among WLHIV. Until now, data on the burden of HR-HPV/HTLV-1 co-infection among WLHIV in Kenya was scant. The research team set out to fill this information gap by determining the prevalence of this co-infection among WLHIV on antiretroviral therapy (ART) at Kenyatta National Hospital (KNH), Kenya’s national referral hospital.
The Study and Its Findings
The cross-sectional study involved 647 WLHIV on ART, with study nurses collecting cervical samples for HPV genotyping and HTLV-1 DNA detection. It revealed that the HTLV-1 positivity rate among WLHIV was 3.1% overall, rising to 7.6% among those with HR-HPV. A significant finding was that WLHIV with HR-HPV 31 had the highest proportion of HR-HPV/HTLV-1 co-infection at 31.6%. In contrast, those with HR-HPV 39 had the lowest proportion of co-infection, standing at 7.1%. The research also found that co-infections were associated with specific demographic and behavioural factors. Participants with HR-HPV/HTLV-1 co-infections were typically older than those without co-infections. The study also noted that many women with HR-HPV/HTLV-1 co-infections had their sexual debut before 18. Furthermore, women co-infected with HR-HPV/HTLV-1 were diagnosed with HIV at an older age, generally ≥ 35 years, compared to those without co-infections.
The Implications
The research presents important data that could contribute to disease prevention and control efforts in Kenya. By uncovering the links between age, sexual debut, HIV diagnosis age, and HR-HPV/HTLV-1 co-infections, this study could inform strategies to curb the spread of these infections among WLHIV. While the study contributes crucial to understanding the prevalence of HR-HPV/HTLV-1 co-infections among WLHIV in Kenya, it also underscores the need for more extensive research in this area. Understanding the complexities of these co-infections could lead to more effective public health interventions, not just in Kenya but in other regions of the world where similar patterns may be present.
To read the entire journal article click here
- Log in to post comments